New Data Highlights Positive Trends in AHCCCS’ Continued Efforts to Combat Medicaid Fraud
CONTACT: PIO@azahcccs.govFOR IMMEDIATE RELEASE
PHOENIX – The Arizona Health Care Cost Containment System (AHCCCS) released new data showcasing the impact of the agency’s actions in response to sober living fraud within Arizona’s Medicaid program.
“While there is still work to be done, this data reflects that our efforts to combat fraud are working,” said Carmen Heredia, cabinet executive officer of AHCCCS. “We have transformed AHCCCS into a new agency that puts our members first and always strives to get them the help they need. We will continue our work to address this issue and prevent future fraud schemes with appropriate and necessary actions.”
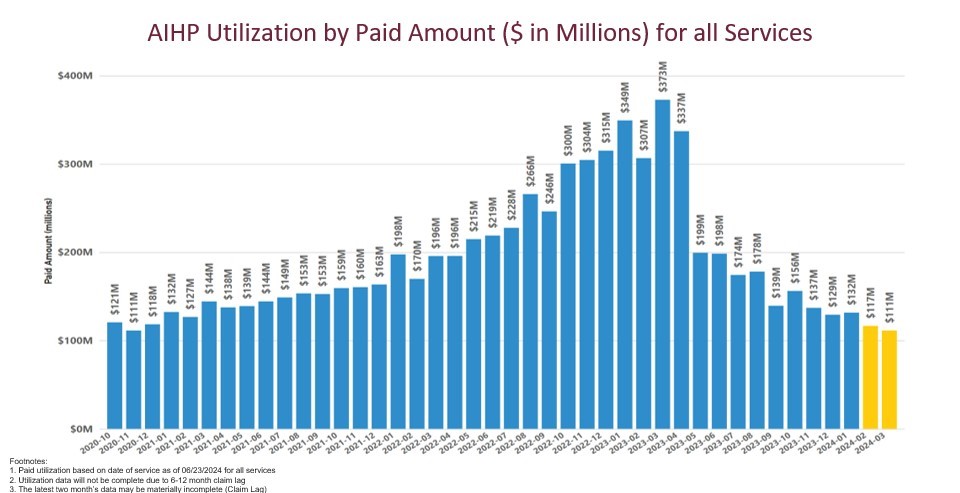
Graph #1 details the AIHP monthly paid amount for all services for the time period October 2020 to March 2024 is included in this release. This data was identified as of 6/23/2024.
Similarly, in Graph #2, the AIHP monthly utilization represented on a Per Member Per Month (PMPM) basis is displayed for the time period October 2020 to March 2024. This data was identified as of 6/23/24.
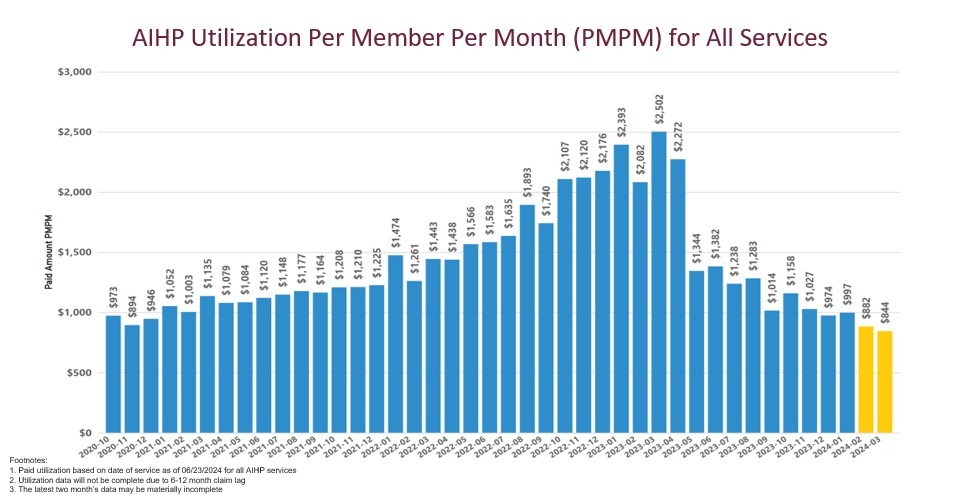
Please note, the last two months are highlighted yellow to indicate that those months may represent incomplete utilization due to the claims lag.
AHCCCS continues to closely monitor the AIHP provider network and the agency is confident the program’s network continues to have the appropriate capacity to ensure quality care and ongoing access to necessary services.
AHCCCS continues to monitor the provider network and those providers who are on Pre–Payment Review to ensure members do not experience a barrier to care. For example, as of this month, only 1.08% of Behavioral Health Residential Facilities (BHRFs), 16.85% of Behavioral Health Outpatient Clinics, and 4.70% of Integrated Clinics are on Pre-Payment Review.
Please visit www.azahcccs.gov/soberlivingfraud to learn more about AHCCCS’ efforts to combat fraud within Arizona’ Medicaid program.

