Behavioral Health Contracts
ACC-Regional Behavioral Health Agreements (ACC-RBHA) Contracts and Service Delivery
On October 1, 2022, AHCCCS updated its contracts with ACC health plans for health insurance coverage for individuals with a Serious Mental Illness (SMI) designation. In November of 2021, AHCCCS awarded select ACC health plans expanded contracts effective October 1, 2022. AHCCCS posted this announcement on its News and Updates web page.
Contract Expansion FAQs for Members, 2/22/2022
Contract Expansion FAQs for Providers, 2/22/2022
Changes in Service Delivery for Members with an SMI Designation

- RBHA to ACC-RBHA Name Change - Services are now provided by contracted health plans known as AHCCCS Complete Care Contractors with Regional Behavioral Health Agreements (ACC-RBHAs).
- New ACC-RBHA in the North Geographic Service Area (GSA) - The awarded ACC-RBHAs are Mercy Care in the Central GSA, Arizona Complete Health-Complete Care Plan in the South GSA, and Care1st Health Plan in the North GSA. Members in the North GSA, transitioned to Care1st Health Plan on October 1, 2022.
- GSA Alignment – The GSAs are now aligned to match the ACC and ALTCS/EPD GSAs.
- Single Statewide Crisis Vendor – Crisis services are available to any Arizona resident, regardless of health insurance coverage. If you or someone you know is experiencing a behavioral health crisis, please call one of the national or local crisis lines listed on the AHCCCS Crisis Hotline web page. See Frequently Asked Questions about the crisis system.
- Behavioral Health Service Delivery for American Indian/Alaska Native Members with an SMI Designation – As of October 1, 2022, AIHP has integrated physical and behavioral health services for American Indian/Alaska Native members. See Frequently Asked Questions about this change.
Behavioral Health Integration
Overview
In Arizona, behavioral health has historically been a carved out benefit which has been separately managed by Regional Behavioral Health Authorities (RBHAs). Because of this structure, up to four different health care systems might be necessary for an individual with a serious mental illness (SMI) to obtain health care: the AHCCCS acute health plan for physical health services; the RBHA for behavioral health services; Medicare for, persons with SMI who are dually eligible for both Medicaid and Medicare; and Medicare Part D for medications.
Navigating the complex health care system is one of the greatest barriers to obtaining medically necessary health care. For Arizonans with SMI, obtaining needed health care has been challenging and further complicated by concerns around poor medication management and stigma, sometimes causing many individuals to forgo physical health care. Because many persons with SMI also experience co-morbidities, management of chronic diseases like diabetes or hypertension has also been poor.
To help address these issues, AHCCCS collaborated with behavioral health partners to create a more streamlined system that reduces barriers to care for members and also increases accountability of the RBHA for managing the “whole health” of persons with SMI. To carry out this new approach, RBHAs manage the delivery of physical health services, in addition to behavioral health services, to increase member engagement in obtaining medically necessary physical health services.
Maricopa County
On April 1, 2014, approximately 17,000 members with Serious Mental Illness in Maricopa County were transitioned to a single plan, Mercy Maricopa Integrated Care, to manage both their behavioral and physical health care needs. On October 1, 2015, this model will be launched statewide through contracts with Health Choice Integrated Care in Northern Arizona and Cenpatico Integrated Care in Southern Arizona. For more information please see the resource links below.
Greater Arizona Integration
To enhance care coordination and broaden accessibility of health care through AHCCCS, members determined to have a serious mental illness (SMI) who do not reside in Maricopa County will be enrolled in one health plan beginning October 1, 2015 for both their physical and behavioral health care needs. These members will be reassigned to one of the integrated health plans (Regional Behavioral Health Authorities (RBHAs) listed below, depending on where they live. Letters have been sent to those members whose enrollment will change to one of the integrated health plans to inform them of their new enrollment.
Members residing in the following Counties will be receiving physical and behavioral health services from Cenpatico Integrated Care beginning October 1, 2015: Cochise, Greenlee, La Paz, Pima, Pinal, Yuma, Santa Cruz, Graham and zip codes 85542 and 85192.
Members residing in the following Counties will be receiving physical and behavioral health services from Health Choice Integrated Care beginning October 1, 2015: Apache, Coconino, Mohave, Navaho, Yavapai and Gila (except zip codes 85542 and 85192).
The Future of RBHA Service Delivery
AHCCCS has made major decisions regarding the future of RBHA service delivery, including the intention to expand the provision of services for at least one ACC plan in each GSA utilizing a Competitive Contract Expansion for the provision of integrated services for Title XIX/XXI eligible individuals determined to have SMI. The effective date for this change will be October 1, 2022
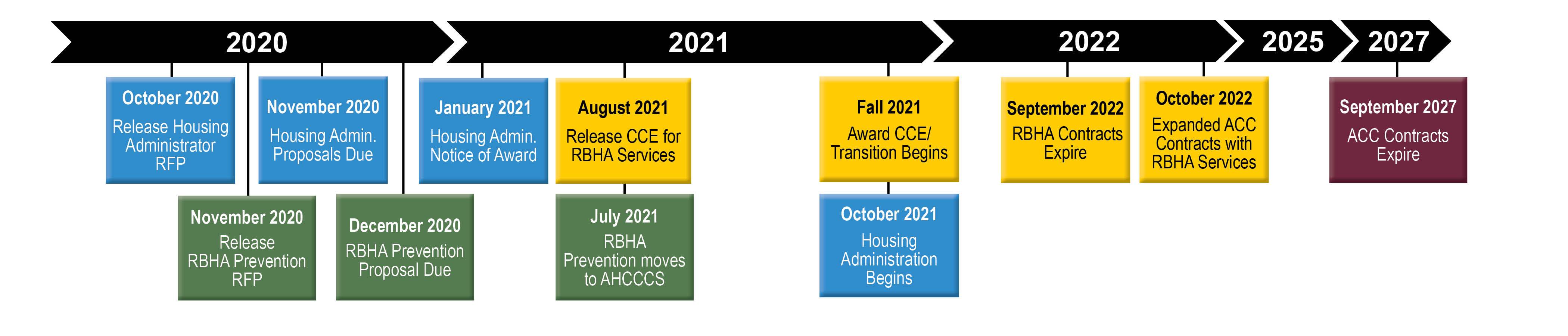
Anticipated Timeline for Competitive Contract Expansion/ Request for Proposal (RFP) Activities
AHCCCS anticipates the timeline for Competitive Contract Expansion/ RFP activities may be as follows:
American Indians
Today, American Indian members have some unique choices for Medicaid service delivery. The American Indian Health Program (AIHP) is a fee for service program delivered through AHCCCS that is responsible for integrated care for American Indian child and adult members who select AIHP and who have not been determined to have SMI. Integrated care services include both physical and behavioral health services, including services related to a CRS condition. American Indians not determined to have SMI can choose to enroll as follows:
- In an ACC Plan to receive both physical health services and behavioral services,
- In AIHP for physical and behavioral health services, or
- In AIHP for physical health services and receive behavioral health care coordination services from a Tribal RBHA (TRBHA) when available.
American Indian members who are determined to have SMI are assigned to the RBHA for all services but also have a choice of staying with the RBHA or selecting AIHP for physical health services and the RBHA or TRBHA (when available) for provision of behavioral health services. American Indian members determined to have SMI are also currently permitted to be enrolled in the ACC Plan for physical health services and the TRBHA for provision of behavioral health services. or to opt out of the RBHA as specified in ACOM Policy 442 to be served by the ACC Plan for physical health services and the RBHA for behavioral health services. American Indian members can always access services from IHS/638 facilities at any time regardless of enrollment.
AHCCCS is engaging stakeholders around important system design questions and decisions that need to be made for American Indian members being served by the RBHAs and TRBHAs. Decisions need to be made regarding American Indian members continuing to have choice of enrollment with portions of their services delivered through managed care, AIHP, RBHAs and TRBHAs. The alternative is to implement change in choice for individuals determined to have SMI to be consistent with the choices for child and adult members not determined to have SMI, allowing integrated options to enroll as follows:
- In an ACC Plan to receive both physical and behavioral services, non-TXIX services tbd, or
- In AIHP for physical, behavioral and other non-TXIX supplemental services, or
- In AIHP for physical health services and receive behavioral health care coordination services from a Tribal RBHA (TRBHA) when available.
Stakeholder Feedback
In order to begin to engage stakeholders around important system design questions and decisions that need to be made in order to best provide these critical services to vulnerable populations, AHCCCS released a RBHA Services RFI in February 2019. In addition, AHCCCS began presenting Community Forums in April 2019 and collected surveys to gather feedback on these changes. Additional forums and opportunities for community feedback will be posted on the Community Forums web page.
High level feedback to date from 21 written RFI responses, primarily from providers and health plans includes:
- Approximately half of respondents support more than one health plan having responsibility for managed care service delivery to individuals determined to have SMI living in large urban areas and half support continuing with a single health plan in each GSA.
- Most service providers support a single health plan serving individuals determined to have SMI to maintain the stability of the delivery system and focus on the unique needs of the members.
- Almost all respondents support a single ACC Plan or outside (non-ACC Plan) entity, either by region or statewide, having responsibility for Non-Title XIX services.
- Most respondents support continuing the current opt out processes to receive physical health services through a different health plan.
- Approximately 70 percent of respondents support allowing requested administrative SMI decertification for members that have not received services in two years.
- All respondents recognize tribal sovereignty and the need for tribal involvement in any decisions affecting tribal choice and services. All recognize the need for tribal expertise with any ACC Plan or non-ACC vendor administering services.
- Almost all respondents support a single entity responsible for first 24 hours of crisis, and some support a single statewide entity while others support one entity per GSA in order to ensure recognition of regional differences.
- Respondents support more AHCCCS involvement monitoring crisis services and vendors.
- All respondents stress the need to start early with this process and have significant education and stakeholder engagement.
- Most respondents support a single 211 number for crisis services statewide.
- The majority of ACC Plans that are not also RBHAs support a single statewide housing contractor, while the RBHAs advocated for housing to remain with the ACC Plans selected to serve individuals determined to have SMI in each GSA.
- Most service providers recommended a third party contractor take over responsibility for housing.
- Respondents indicated the need for the ACC Plans that serve individuals determined to have SMI be required to ensure that their Office of Individual and Family Affairs include a specialized focus on these individuals ensuring the plan employs a recovery and resiliency based approach to treatment and care management for members.

